[ad_1]
That is the subtitle of an NBER working paper by Charles Gray, Abby E. Alpert & Neeraj Sood. The writer look at latest mergers between pharmacy profit managers (PBMs) and well being insurers. On the one hand, integration could useful to shoppers. It may: (i) enhance operational efficiencies, and (ii) higher align PBM incentives with these of the well being plan (e.g., higher accounting for medical prices offsets). However, the authors additionally notice that there are two pathways by means of which the combination may depart shoppers worse off: (i) enter foreclosures and (ii) buyer foreclosures.
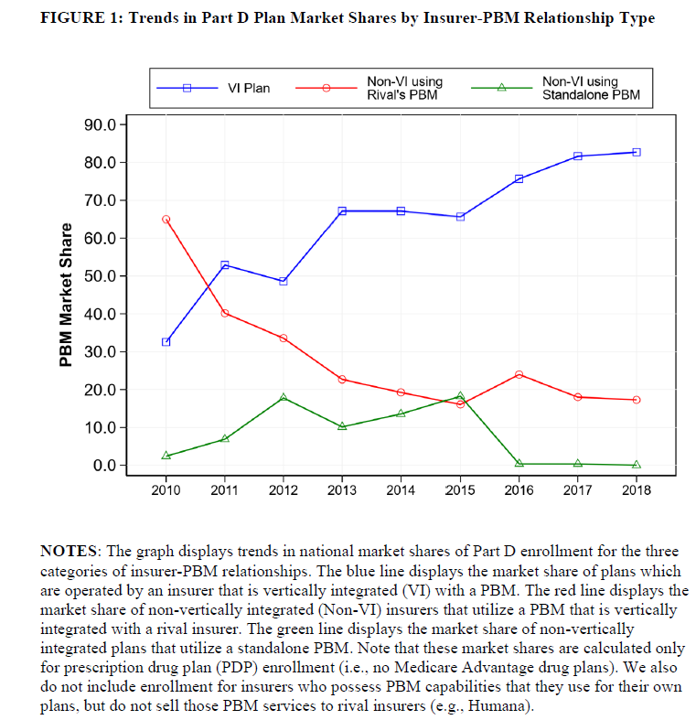
Input foreclosures happens when a PBM owned by an insurer will increase the prices or reduces the standard of its companies supplied to insurers who compete with its mum or dad insurer. For instance, the PBM may go by means of a bigger share of producer rebates to its mum or dad insurer than it passes by means of to rival insurers. The diploma of enter foreclosures will depend on the extent of competitors within the PBM market. If PBM markets have many opponents, then enter foreclosures is much less probably as rival well being plans experiencing enter foreclosures can swap to one among many standalone PBMs. However, if PBM markets are extremely concentrated then enter foreclosures is extra probably as rival plans have restricted choices to modify to a different PBM. Customer foreclosures, against this, happens when the downstream agency of a merged entity now not purchases inputs from its upstream opponents. For occasion, when an insurer and PBM consolidate, the insurer’s well being plans will at all times use companies from its personal PBM, thus lowering the potential variety of purchasers for standalone PBMs. The discount within the potential buyer base may finally lead standalone PBMs to exit the market which might additional improve the focus of PBMs.
The authors use quite a lot of completely different datasets together with (i) publicly out there CMS PDP Landscape file datasets on Medicare Part D plan traits and enrollment (2010-2018), (ii) CMS Part D Contract and Enrollment Data include data on plan’s annual enrollment, and (iii) Decision Resources Group
(DRG) Managed Market Surveyor (MMS) (2010-2018) to establish which PBM every Part D plan makes use of.
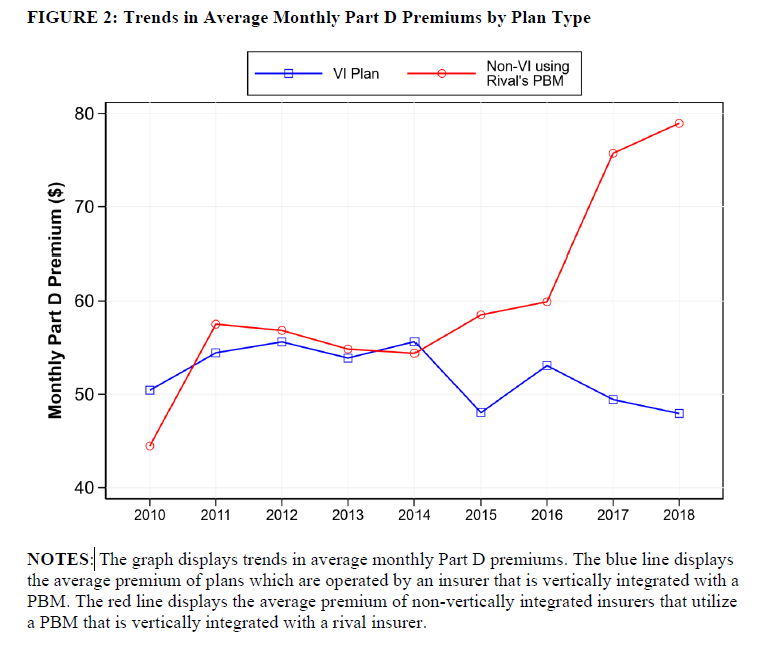
Then, they carry out a difference-in-differences (DD) evaluation wanting on the Part D market earlier than and after a big 2015 insurer-PBM merger (UnitedHealth-Catamaran), which the authors declare “eliminated the last significant standalone PBM and shifted more insurers into contracts with vertically integrated PBMs.” The pre-post evaluation compares modifications in premiums for vertically built-in plans (i.e., plan owns their very own PBM) in comparison with non-vertically built-in plans.
Using this strategy, the authors discover that:
…nonvertically insurers skilled premium will increase of 36% when in comparison with vertically built-in insurers. These findings are in keeping with vertically built-in PBMs participating in enter foreclosures. Specifically, a vertically built-in PBM had a bigger incentive to lift prices for rivals when these rivals misplaced the power to substitute to a standalone PBM.
The figures under present that (i) vertically built-in plans started to dominate the market and (ii) costs for non-vertically built-in plans elevated greater than for vertically built-in plans.