[ad_1]
Back in July, I supplied an overview of the Enhancing Oncology Model (EOM). Today I construct upon that submit focusing largely on CMS’s EOM’s Payment Methodology. I exploit a Q&A format as nicely.
What is the aim of EOM?
According to CMS “EOM is a CMMI alternative payment model designed to advance health equity, promote better care coordination, improve access to care, reduce costs, and improve outcomes for Medicare fee-for-service (FFS) beneficiaries with cancer who receive chemotherapy.”
Which most cancers sorts are eligible for EOM included?
There are seven most cancers sorts eligible for EOM: (i) breast, (ii) persistent leukemia, (iii) lung, (iv) lymphoma, (v) a number of myeloma, (vi) prostate most cancers, and (vii) small gut / colorectal most cancers.
Note that low-risk breast most cancers (i.e., long-term oral endocrine chemotherapy) and low-intensity prostate most cancers (indicated by androgen deprivation and/or anti-androgen remedy with out chemotherapy) usually are not included in EOM.
Does EOM solely think about chemotherapies?
No! Although all of the CMS language makes use of the time period “chemotherapy” continuously, EOM Initiating Therapies embody not solely conventional chemotherapies (e.g., azacitidine, carboplatin, decitabine), however contains immuno-oncology remedies (e.g., nivolumab, pembrolizumab) and focused therapies (e.g., bevacizumab, osimertinib, sorafenib? A full checklist is out there on the EOM web site right here.
Cell and gene therapies–which CMS calls n Adoptive Cell Transfer (ACT) remedy–are excluded from the EOM program. For occasion, CAR T-cell therapies are excluded from the EOM program.
How lengthy are EOM episodes?
6 months.
Episodes begin at a “trigger event” which is the initiation of a Part B or Part D anti-cancer remedy. Beneficiaries who proceed to obtain chemotherapy after finishing a six month episode provoke a brand new episode. Note, nevertheless, that “There is no requirement that a chemotherapy-free period exist before the beginning of any episode.” The deal with the shortage of a ‘clean period’ earlier than the set off occasion, CMS depends on threat adjustment.
How are episodes assigned to doctor follow teams?
This relies on the oncology doctor group follow that both (i) supplied the primary analysis and administration (E&M) service through the 6 month efficiency interval so long as they supplied a minimum of 25% of E&M companies within the episode, or (ii) the PGP with the plurality of E&M companies if the preliminary PGP didn’t attain the 25% threshold.
What varieties of funds can physicians group practices (PGPs) obtain?
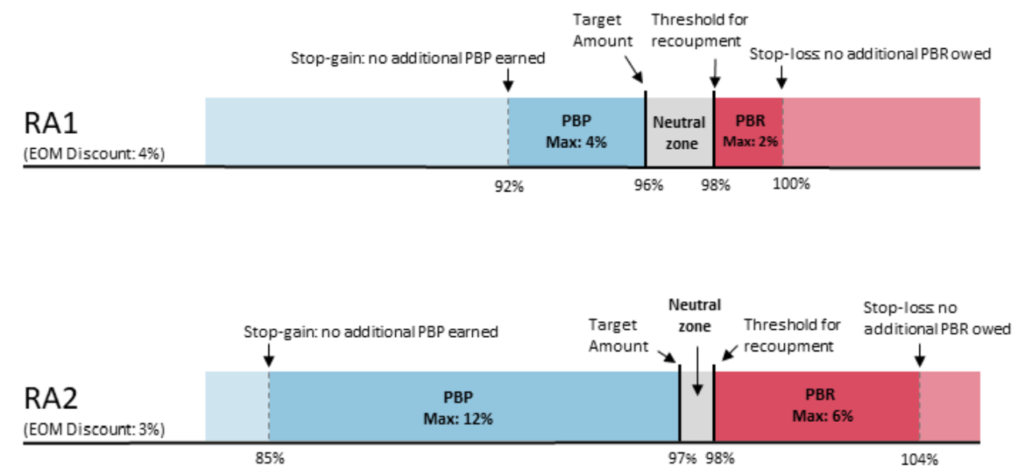
Practices obtain the usual Medicare FFS billing. In addition, EOM has the choice to incorporate a Monthly Enhanced Oncology Services (MEOS) fee, which might be considered a capitation fee. Base MEOS funds are $70 monthly however enhance to $100 monthly for dual-eligible beneficiaries. Based on therapy price and high quality, PGPs have two-sided threat: high-quality/low price PGPs can earn a retrospective performance-based fee (PBP), however low-quality/high-cost PGPs can owe a retrospective performance-based recoupment (PBR).
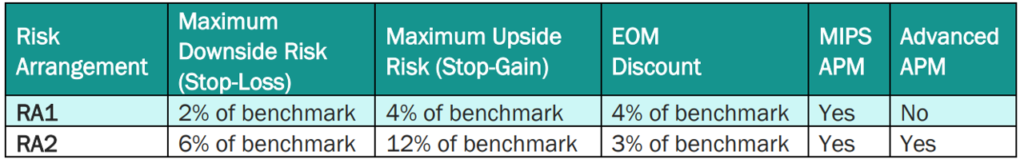
PBP and PBRs rely on the danger mannequin chosen. By default, EOM contributors and swimming pools are in RA1 until they request to be in RA2. The fee specs for RA1 and RA2 are beneath. RA1 requires PGPs to satisfy a bigger goal low cost (4%) however has a 2% most draw back threat; RA2 requires a smaller low cost (3%) however PGPs are accountable for extra optimistic and unfavourable threat (most 6% draw back threat). By default, EOM contributors and swimming pools are in RA1 until they request to be in RA2.
What kind of expenditures are included in an episode?
All Medicare Part A and Part B FFS expenditures (funds) and sure Part D expenditures are counted as a part of the episode price. Specifically, EOM episodes solely embody the Low-Income Cost Sharing Subsidy (LICS) quantity and 80 % of the Gross Drug Cost above the Catastrophic (GDCA) threshold. All different Part D expenditures usually are not included in an EOM episode as a result of they’re paid on a capitated foundation by Part D plans.
How does EOM account for outlier episodes and variations in affected person traits?
To cut back the probability that just a few very excessive or very low price episodes will result in a poor efficiency rating, CMS winsorizes episode expenditures on the fifth and ninety fifth percentiles.
Additionally, CMS threat adjusts episode prices based mostly on components reminiscent of demographics (i.e., age, intercourse), revenue (i.e., twin eligibility, Part D LIS eligibility), comorbidities (autoimmune issues, COPD, dementia, endocrine issues, heard illness hematologic illness, hypertension), rely of different HCCs, receipt of particular companies (i.e., cancer-directed surgical procedures, bone marrow transplant, radiation), institutional standing, participation in a scientific trial, prior chemotherapy use, and episode size (e.g., if died or disenrolled)
weight problems. Risk adjustment relies 50% on nationwide cancer-specific price predictions and a mixture of regional and PGP particular price estimates with bigger PGPs having extra weight on their historic information and smaller PGPs having extra weight on regional price predictions.
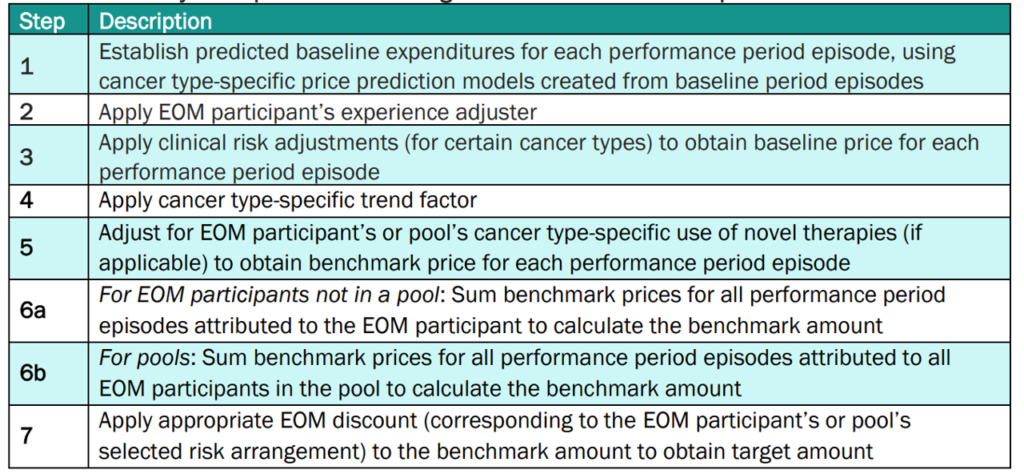
More particulars on how CMS calculates the goal quantities for EOM participant PGPs is beneath.
Does EOM account for tumor stage or tumor mutations?
Yes, however crudely. There is a scientific adjuster if the affected person ever had metastatic illness (at the moment solely used for breast, lung and small gut/colorectal cancers), and a single biomarker is adjusted for (HER2+ sufferers with breast most cancers).
How does EOM take care of new remedies?
EOM might doubtlessly de-incentivize the usage of clinically useful however excessive price remedies. To not unduly disincentivize innovation, EOM features a new remedy adjustment the place oncology medicine are thought of “new” for two years from FDA approval for that particular indication.
Does EOM account for high quality of care?
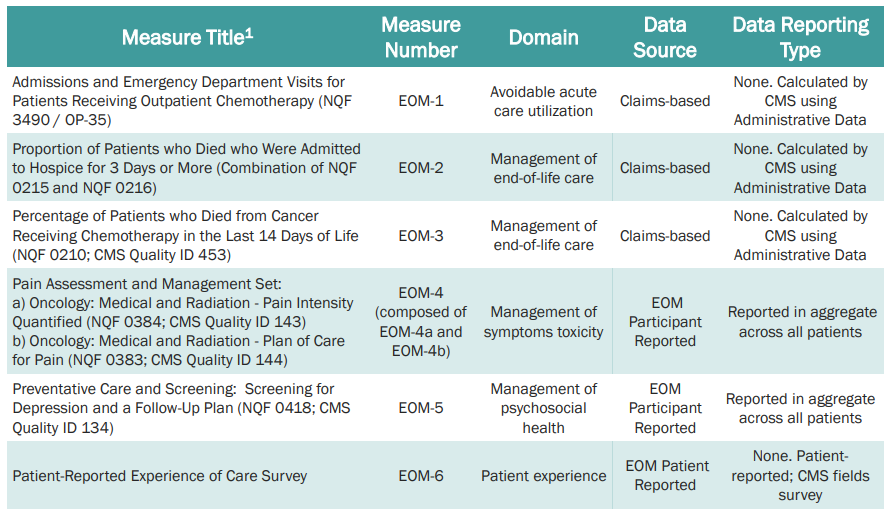
Somewhat. EOM does this by way of Aggregate Quality Score (AQS). In quick, PGPs are solely eligible to obtain bonuses in the event that they meet a minimal threshold on the AQS.
Quality of care contains sure actions (24/7 entry to care, affected person navigation, documented care plan, following scientific tips, conducting health-related social wants screening, and use of licensed digital well being data expertise (CEHRT). The particular high quality measures are listed beneath based mostly on CMS’s Quality Strategy Webinar from August 25, 2022.
For extra particulars on EOM because it evolves, see the CMS’s EOM web site.
[ad_2]
