[ad_1]
In a latest examine posted to the medRxiv* preprint server, researchers in Australia and Switzerland evaluated the prevalence of extreme acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants of concern (VOCs) in community-based settings of the United States (US).
The continuous emergence of SARS-CoV-2 VOCs has elevated coronavirus 2019 (COVID-19) mitigation difficulties. Omicron sub-VOC BA.1 emergence was adopted by the circulation of Omicron sub-VOCs BA.2, BA.5, and BA.2.75. In addition, BA.5 is reported to have better immune-evasiveness than its mum or dad (BA.2) VOC on account of spike (S) protein receptor-binding area (RBD) mutations and better TMPRSS2 use.
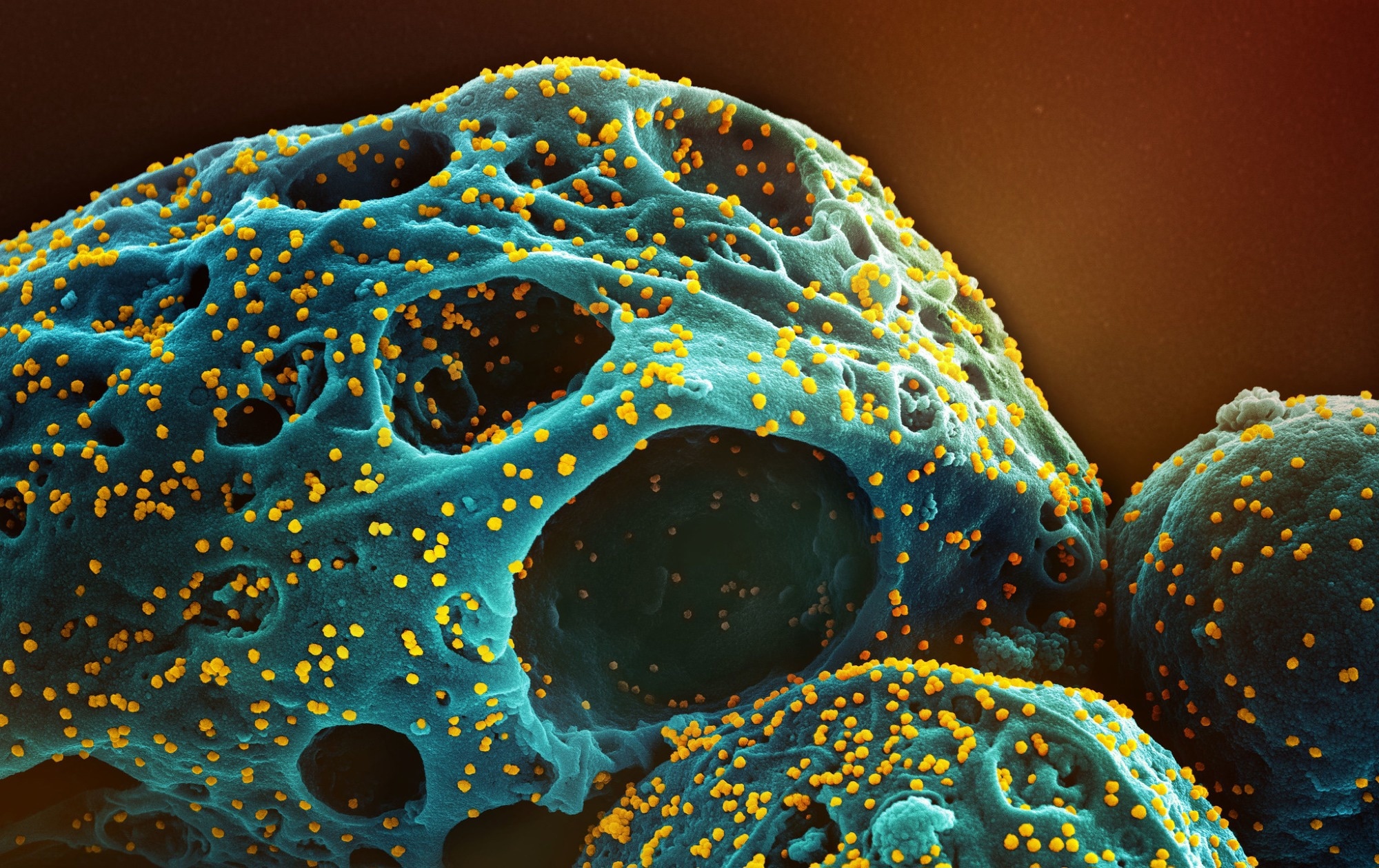 Study: Emergence and antibody evasion of BQ and BA.2.75 SARS-CoV-2 sublineages within the face of maturing antibody breadth on the inhabitants stage. Image Credit: NIAID
Study: Emergence and antibody evasion of BQ and BA.2.75 SARS-CoV-2 sublineages within the face of maturing antibody breadth on the inhabitants stage. Image Credit: NIAID
About the examine
In the current examine, researchers evaluated SARS-CoV-2 VOC prevalence in US communities.
The staff monitored the efficiency and breadth of antibody neutralization responses to a number of rising VOCs at two ranges. Blood samples have been obtained from COVID-19 vaccinees and convalescents to map VOC responses to monoclonal antibodies corresponding to Evusheld (cilgavimab and tixagevimab mixture) and Sotrovimab. To assess neutralization response maturation, 37 sequential immunoglobulin G (IgG)-derived serum pool batches of >420,000 people have been analyzed between August 2021 and June 2022.
VOC isolation (together with BQ.1.1, XBB.1, and BR.2.1 (+R346T), BL.1 BR.2.1 (346R), BA.4.6 and BA.5) and ex vivo entire genome sequencing of SARS-CoV-2 obtained from nasopharyngeal swabs have been carried out all through 2022. Transmembrane serine protease 2 (TMPRSS2) use by VOCs was evaluated utilizing HAT-24 cells, and the results of S protein mutations on TMPRSS2 use have been evaluated. SARS-CoV-2 titers have been evaluated by quantitative polymerase chain response (qPCR) evaluation. To decide whether or not the adjustments in breadth and efficiency have been related to vaccination versus BA.1 an infection, the staff plotted imply neutralization titers and breadth with three key comparators: month of plasma assortment, VOC breadth, and reported SARS-CoV-2 an infection instances.
Further, anti-nucleocapsid (N) protein IgG titers have been decided. The staff examined neutralizing responses of sera from the VIIM (vaccine, an infection, and immunology collaborative analysis) cohort and the ADAPT (Australians’ drug use: adapting to pandemic threats) cohort of Australian people. VIIM cohort samples have been obtained in September 2022, and ADAPT cohort samples have been obtained between March and September 2022. Whole S protein dwell cell assays have been carried out, and the phenotypes of antibody evasion and SARS-CoV-2 entry MODES have been characterised. To decide BA.5 phenotype tropism, the staff in contrast Delta, BA.2, and BA.5 infections in main human bronchial- and alveolar epithelial cultures differentiated on the air-liquid interface (ALI).
To monitor the phenotype of rising VOCs past antibody evasion, endpoint titers of 188 main swabs have been decided between October and November 2022. Donor people have been grouped as follows (i) 3.0-dose Pfizer messenger ribonucleic acid (mRNA) vaccinees with a 6.0 month-post-vaccination interval; (ii) 3.0-dose Pfizer mRNA vaccinees with breakthrough BA.2/BA.5 infections (between June and August 2022); (iii) 4.0-dose Pfizer vaccinees, with the newest dose within the final 3.0 months; and (iv) donors contaminated between March and August 2020 who obtained 3.0 vaccinations late 2021 onward and a Pfizer vaccine booster within the preliminary days of 2022.
Results
The staff remoted A.2.2 clade (ancestral) VOC, Delta VOC, emerged Omicron BA.1 sub-VOC, BA.2 sub-VOC and Omicron BA.5 sub-VOC, and the yet-to-emerge Omicron BL.1 sub-VOC, BQ.1.1 sub-VOC, BQ.1.2 sub-VOC, XXB.1 sub-VOC, and Omicron BR.2.1 sub-VOC. Elevated antibody breadth was noticed in rising VOCs. BQ.1.1, XBB.1, and BR.2.1 have been extremely immune-evasive (with the best variety of RBD mutations and 18-fold to 20-fold decrease neutralization than A.2.2 neutralization throughout all examine cohorts). The three immune-evasive VOCs have been proof against Evusheld; nevertheless, solely BQ.1.1 confirmed Sotrovimab resistance, with 58-fold decrease binding antibody titers than the ancestral clade).
The convergence of S protein polymorphisms throughout rising lineages considerably decreased the efficiency and breadth of neutralization responses throughout all cohorts. Samples obtained in October have been enriched for BA.5-derived lineages, and people in mid-November have been enriched by BA.5 mum or dad (e.g., BQ.1)- or BA.2.75 parent-derived lineages (particularly BR.2.1 VOC with attribute S67F mutation within the open studying body 8 (ORF8). BA.2.75- and BA.5-derived lineages confirmed mutations in school I, II, and III antibody websites throughout the RBD, corresponding to L452R/M, R346T, N460K, F486V/I, F490S, and K444R/T.
Lowered anti-N IgG ranges in comparison with neutralization titers have been noticed, indicating that COVID-19 vaccination and no an infection contributed to enhanced breadth and neutralization. Contrastingly, A.2.2 neutralization titers and anti-N IgG titers peaked in February, related to BA.1 sub-VOC peak decision throughout January of 2022. Concomitant uptake of vaccines and BA.1 infections led to elevated BA.1 sub-VOC, BA.2 sub-VOC, BA.5 sub-VOC, and Omicron BL.1 sub-VOC neutralization.
Anti-N titers elevated after the BA.2 peak, and thus, the growing breadth of neutralization responses throughout the examine interval could signify two predominant immune occasions in late 2021-early 2022, i.e., third-dose vaccinations and Omicron BA.1 infections. BQ lineages (with excessive infectivity to particle ratios and better fusogenicity) utilized TMPRSS2 greater than BA.2.75-derived lineages, BA.1 and BA.2. BA.5 confirmed excessive TMPRSS2 use (however lower than Delta), leading to a progress benefit throughout pulmonary epithelial cells. Delta confirmed greater reductions in titers within the presence of Nafamostat.
Overall, the examine findings confirmed that BQ-derived sub-lineages effectively evade neutralization responses and maintain an outgrowth benefit of TMPRSS2 utilization at ranges similar to BA.5.
*Important discover
medRxiv publishes preliminary scientific reviews that aren’t peer-reviewed and, due to this fact, shouldn’t be thought to be conclusive, information scientific apply/health-related conduct, or handled as established data.
[ad_2]
