[ad_1]
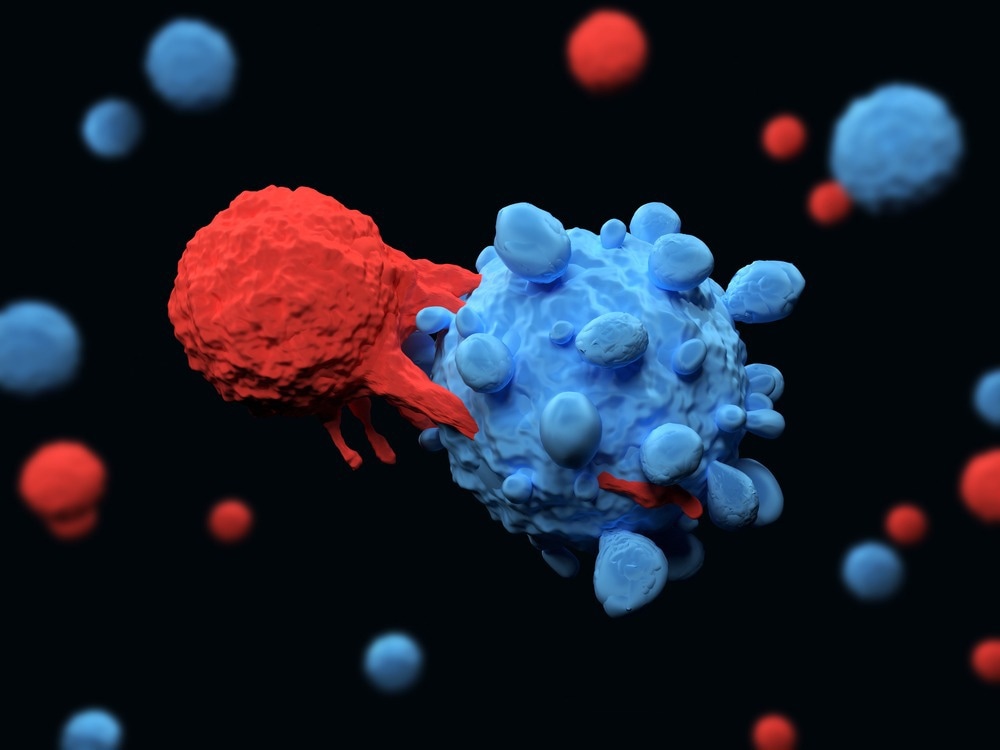
In a current research printed in Frontiers in Immunology, researchers assessed the efficacy of chimeric antigen receptor (CAR) T-cells within the immunotherapy of colorectal most cancers (CRC).
Background
CAR T-cells are a novel cell-based immunotherapy towards most cancers that’s developed genetically. The software of CAR T-cells has reworked the remedy of hematological cancers. Before this remedy will be modified to deal with stable tumors, reminiscent of colorectal most cancers, intensive analysis is important. CAR T-cell remedy for colorectal most cancers is in its infancy, and there’s scarce scientific knowledge out there. Significant drawbacks of CAR T-cell remedy for colorectal most cancers embrace vital toxicity, relapses, and an impenetrable tumor microenvironment.
Biological options of CAR T-cell engineering
In the current research, researchers assessed the CAR T-cell remedy for colorectal most cancers with respect to present information, recognized obstacles, and future views.
CAR T-cell remedy is a personalised immunotherapy based mostly on autologous or allogeneic artificial CAR-expressing T-cells which have been genetically engineered. The CAR molecule consists of extracellular binding moieties, both a tumor-specific antigen (TSA)-sensing factor or a single-chain fragment variable derived from an antibody. There can also be a transmembrane anchor mixed with signaling domains of the T-cell-receptor zeta chain complicated and costimulatory molecules like CD28 and 4-1BB.
CAR T-cell activation arises from the direct and particular identification of tumor antigens by the extracellular area, which ends up in the killing of most cancers cells. T-cells of a affected person are sometimes transduced with gammaretroviral or lentiviral vectors to precise CARs. After CAR T-cells are manufactured ex vivo, the affected person undergoes lymphodepleting chemotherapy, if vital, with subsequent CAR T-cell injection.
CAR T-cells play a promising function within the remedy of CRC
Surgical and chemotherapeutic first-line therapies for sufferers with CRC have lengthy resulted in poor prognoses. The growth of target-selective and efficient medicines was made attainable by a greater comprehension of the processes contributing to tumor growth and proliferation. Although CAR T-cells are glorious candidates towards hematological malignancies, their efficacy towards stable tumors, reminiscent of CRC, stays unverified. Several teams have focused on CAR T-cell biology preclinical analysis to ascertain protected remedy strategies and ensure their effectiveness in CRC.
Epithelial cell adhesion molecule
One of the primary preclinical investigations studied the deadly impacts of epithelial cell adhesion molecules (EpCAM)-directed CAR T-cells. Normal epithelial cells categorical EpCAM, a transmembrane glycoprotein, on their floor. Its overexpression is linked to enhanced cell proliferation, invasion, migration, and metastasis. Extensive peritoneal metastases and ascites formation have been noticed in an in vivo immunodeficient mouse mannequin of late-stage metastatic most cancers amongst people. Repetitive injections of EpCAM-CAR T-cells inhibited the development of peritoneal illness in xenografted mice with tumors.
Carcinoembryonic antigen
Carcinoembryonic antigen (CEA) can also be a goal of anti-CRC CAR T-cells which have been explored. CEA is an immunoglobulin glycoprotein overexpressed in numerous human malignancies, together with colon, lung, gastric, pancreatic, and ovarian cancers. CEA is among the many most vital prognostic and diagnostic tumor indicators and is overexpressed in over 98% of CRC tissue samples. Thus, CEA-targeted therapies have the potential to supply novel CRC remedy strategies. CAR T-cells focusing on CEA have exhibited excellent anticancer exercise in vitro in addition to in vivo, which was significantly enhanced by the addition of interleukins reminiscent of interleukin (IL)-12.
Epidermal development issue receptor
In a xenograft mannequin created by co-inoculation of tumor cells with CAR T cells, a research discovered that EGFRvIII-CAR T-cells mixed with miR-153 fully eradicated the tumor. These findings recommended that miR-153 decreased indoleamine 2,3-dioxygenase (IDO)-1 expression amongst CRC cells and improved the efficacy of CAR T-cell remedy. Therefore, the mixture of IDO1 inhibitors with CAR T-cells has the potential to perform as an efficient remedy for CRC and stable tumors.
Studies have additionally discovered that engineered cells that categorical a CAR that’s able to binding a fluorescein isothiocyanate (FITC) molecule (anti-FITC CAR T-cells) improved the power of CAR T-cells to deal with mice with estimated glomerular filtration fee (eGFR)-positive CRC tumors. In an immunocompromised mouse mannequin, distinctive interactions between anti-FITC CAR T-cells and FITC-labeled cetuximab slowed the development of colon most cancers.
CAR T-cell research for CRC
Ongoing research examine the appliance of CEA-specific CAR T-cells in sufferers with CEA-positive CRC. The purpose is to confirm efficacy and security, in addition to to find out the fitting doses and infusion schedule. Another goal of those investigations is to determine antagonistic results, significantly cytokine launch syndrome. Protocols for administration embrace hepatic and systemic transarterial supply, vascular intervention, and intraperitoneal infusion, whereas the outcomes are awaited.
Also below analysis is a novel combinatorial approach involving human epidermal development issue receptor 2 (HER2)-specific CAR T-cells together with an oncolytic adenovirus (CAdVEC). Oncolytic adenoviruses reproduce and propagate completely inside tumors, augmenting their cytotoxicity, enhancing tumor penetration, and reverting immune suppression. CAdVEC is a modified adenovirus with immunostimulatory parts. Currently, Phase 1 trials are evaluating the efficacy and security of HER2 CAR T-cells mixed with oncolysis.
Conclusion
Overall, the research findings confirmed that CAR T-cells proceed to garner proof supporting their software as a viable immunological methodology of most cancers remedy. This technique has considerably improved affected person remedy in hematological malignancies.
[ad_2]
