[ad_1]
OAKLAND, Calif. — Medi-Cal well being protection kicked in for Antonio Abundis simply when the custodian wanted it most.
Shortly after Abundis transitioned from restricted to full-scope protection in 2022 beneath California’s growth of Medi-Cal to older residents with out authorized immigration standing, he was recognized with leukemia, a most cancers affecting the blood cells. The soft-spoken father of three took the information in stride as his physician stated his blood take a look at recommended his most cancers wasn’t superior. His subsequent steps have been to get extra assessments and formulate a remedy plan with a most cancers staff at Epic Care in Emeryville. But all of that was derailed when he confirmed up final July for bloodwork at La Clínica de La Raza in Oakland and was informed he was not on Medi-Cal.
“They never sent me a letter or anything telling me that I was removed,” Abundis, now 63, stated in Spanish about dropping his insurance coverage.
Abundis is amongst lots of of 1000’s of Latinos who’ve been kicked off Medi-Cal, California’s Medicaid program for low-income folks, as states resume annual eligibility checks that have been paused on the peak of the covid-19 pandemic. The redetermination course of, as it’s recognized, has disproportionately affected Latinos, who make up a majority of Medi-Cal beneficiaries. According to the California Department of Health Care Services, greater than 653,000 of the greater than 1.3 million residents who’ve been disenrolled over eight months establish as Latino. Some, together with Abundis, had solely lately gained protection because the state expanded Medi-Cal to residents with out authorized residency.
The collision of state and federal insurance policies has not solely set off enrollee whiplash however swelled demand for enrollment help as persons are dropped from Medi-Cal, typically for procedural points. Health teams serving Latino communities report being inundated by requests for assist, however on the identical time, a state-sponsored survey suggests Hispanic households are extra doubtless than different ethnic or racial teams to lose protection as a result of they’re much less educated of the renewal course of. They might also wrestle to advocate for themselves.

Some well being advocates are urgent for a pause. They warn that disenrollments won’t solely undercut the state’s effort to cut back the variety of uninsured however may exacerbate well being disparities, significantly for an ethnic group that bore the brunt of the pandemic. One nationwide research discovered that Latinos within the U.S. have been 3 times as prone to contract covid and twice as prone to die of it than the final inhabitants, partially as a result of they have an inclination to reside in additional crowded or multigenerational households and work in front-line jobs.
“These difficulties place all of us as a community in this more fragile state where the safety net means even more now,” stated Seciah Aquino, govt director of the Latino Coalition for a Healthy California, a well being advocacy group.
Assembly member Tasha Boerner, an Encinitas Democrat, has launched a invoice that might sluggish disenrollments by permitting folks 19 and older to maintain their protection routinely for 12 months and prolong versatile pandemic-era insurance policies reminiscent of not requiring proof of earnings in sure instances for renewals. That would profit Hispanics, who make up practically 51% of the Medi-Cal inhabitants in contrast with 40% of the general state inhabitants. The governor’s workplace stated it doesn’t touch upon pending laws.
Tony Cava, a spokesperson for the Department of Health Care Services, stated in an e mail that the company has taken steps to extend the variety of folks routinely reenrolled in Medi-Cal and doesn’t contemplate a pause needed. The disenrollment charge dropped 10% from November to December, Cava stated.
Still, state officers acknowledge extra might be carried out to assist folks full their functions. “We’re still not reaching certain pockets,” stated Yingjia Huang, assistant deputy director of well being care advantages and eligibility at DHCS.
California was the first state to increase Medicaid eligibility to all certified immigrants no matter authorized standing, phasing it in over a number of years: youngsters in 2016, younger adults ages 19-26 in 2020, folks 50 and older in 2022, and all remaining adults this 12 months.
But California, like different states, resumed eligibility checks final April, and the method is predicted to proceed by May. The state is now seeing disenrollment charges return to pre-pandemic ranges, or 19%-20% of the Medi-Cal inhabitants annually, in line with DHCS.
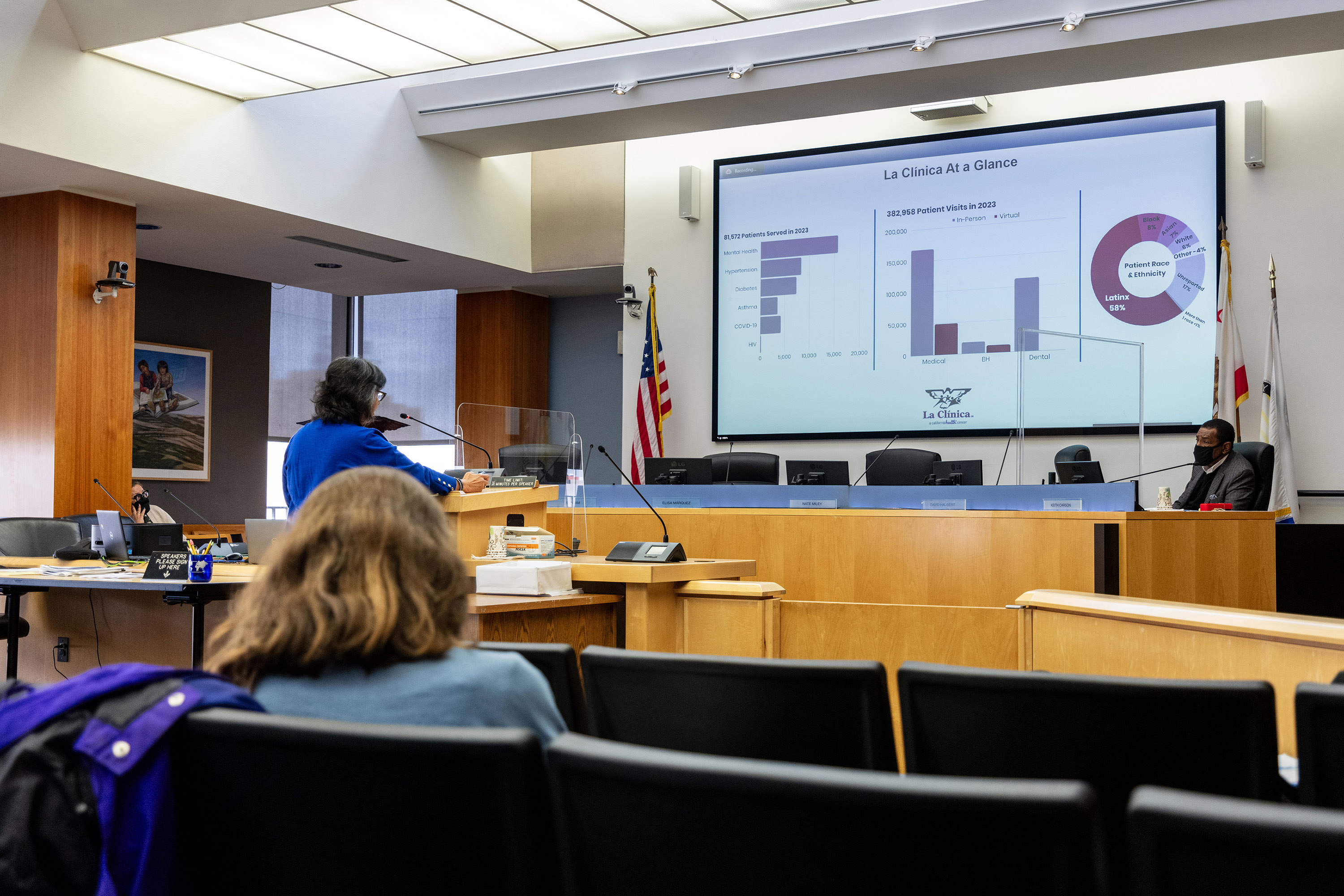
Jane Garcia, CEO of La Clínica de La Raza, testified earlier than the Alameda County Board of Supervisors’ well being committee that disenrollments proceed to pose a problem simply as her staff tries to enroll newly eligible residents. “It’s a heck of a load on our staff,” she informed supervisors in January.

Although many beneficiaries not qualify as a result of their incomes rose, extra have been dropped from the rolls for failing to reply to notices or return paperwork. Often, renewal packets have been despatched to outdated addresses. Many discover out they’ve misplaced protection solely upon looking for medical care.
“They knew something was happening,” stated Janet Anwar, eligibility supervisor at Tiburcio Vasquez Health Center within the East Bay. “They didn’t know exactly what it was, how it was gonna affect them until actually the day came and they were disenrolled. And they were getting checked in or scheduling an appointment, then, ‘Hey, you lost your coverage.’”
But reenrollment is a problem. A state-sponsored survey printed Feb. 12 by the California Health Care Foundation discovered 30% of Hispanic households tried however have been unable to finish a renewal type, in contrast with 19% for white non-Hispanic households. And 43% of Hispanics reported they want to restart Medi-Cal however didn’t understand how, versus 32% of individuals in white non-Hispanic households.
The Abundis household is amongst those that don’t know the place to get their questions answered. Though Abundis’ spouse submitted the household’s Medi-Cal renewal paperwork in October, his spouse and two youngsters who nonetheless reside with them have been capable of keep protection; Abundis was the one one dropped. He hasn’t acquired an evidence for being disenrolled nor been notified find out how to enchantment or reapply. Now he worries he might not qualify on his personal based mostly on his roughly $36,000 annual earnings because the restrict is $20,121 for a person however $41,400 for a household of 4.
It is probably going an eligibility employee may examine if he and his household qualify as a family or help him with signing up for a personal plan that may run lower than $10 a month for premiums on Covered California. The medical insurance trade permits for particular enrollment when folks lose Medi-Cal or employer-based protection. But Abundis assumes he gained’t be capable of afford premiums or copays, so he hasn’t utilized.
Abundis, who first visited a physician in May 2022 about unrelenting fatigue, fixed ache in his again and knees, shortness of breath, and unexplained weight reduction, worries he’s unable to afford medical care. La Clínica de La Raza, the group well being clinic the place he acquired blood testing, labored with him that day so he didn’t should pay upfront, however he has since stopped looking for medical care.
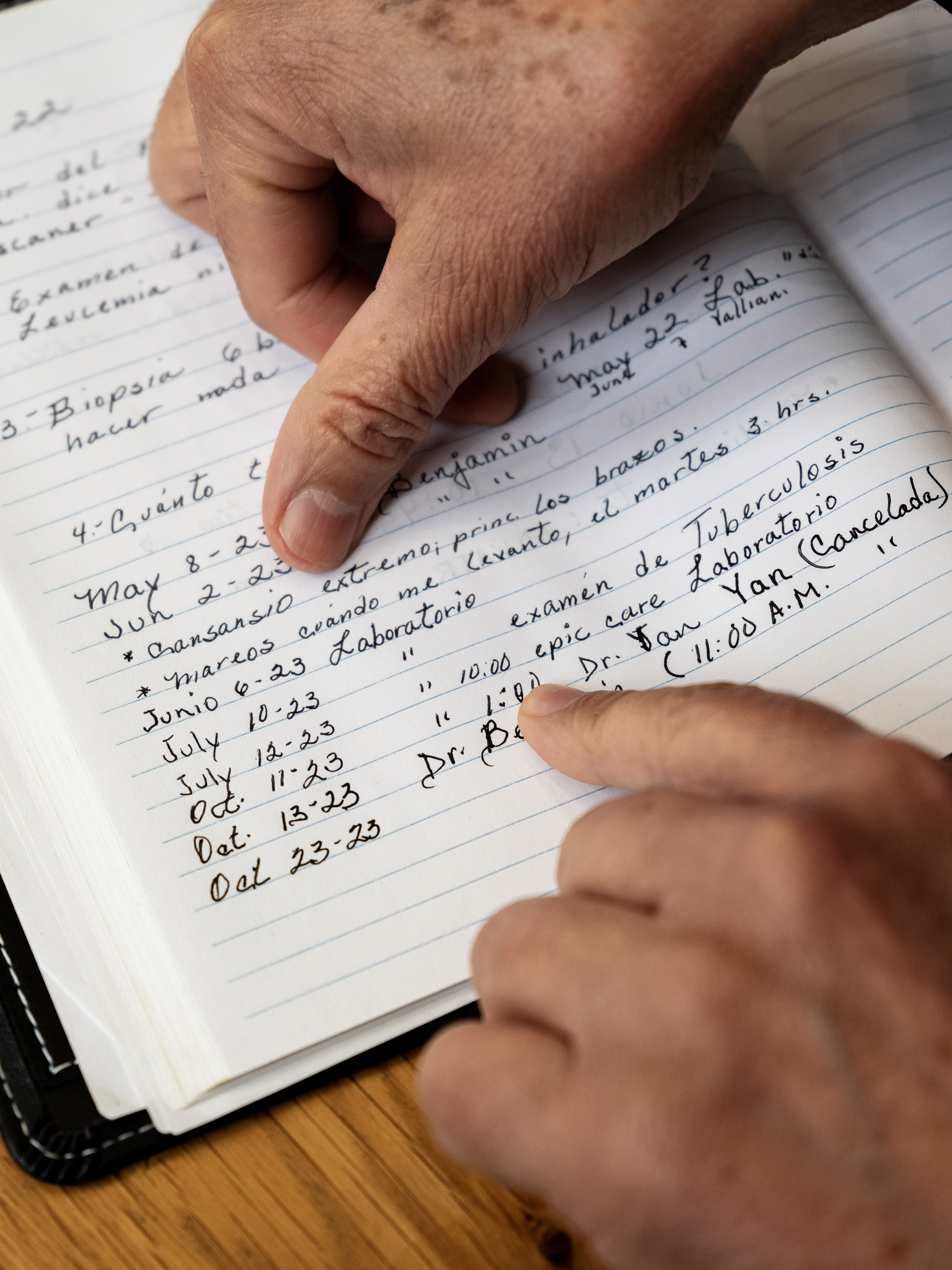
More than a 12 months after his prognosis, Abundis nonetheless doesn’t know which stage most cancers he has, or what his remedy plan must be. Though early most cancers detection can result in a greater likelihood of survival, some kinds of leukemia advance shortly. Without additional testing, Abundis doesn’t know his outlook.
“I’ve mentally prepared,” Abundis stated of his most cancers. “What happens, happens.”
Even those that search assist run into challenges. Marisol, a 53-year-old immigrant from Mexico who lives in Richmond, California, with out authorized permission, tried to reestablish protection for months. Although the state noticed a 26% drop in disenrollments from December to January, the share of Latinos disenrolled throughout that interval remained practically the identical, suggesting they face extra boundaries to renewal.
Marisol, who requested her final title be withheld out of concern of deportation, additionally certified for full-scope Medi-Cal in the course of the state growth to all immigrants 50 and older.
She acquired a packet in December letting her know that her family earnings exceeded Medi-Cal’s threshold — one thing she believed was an error. Marisol’s husband is out of labor attributable to a again harm, she stated, and her two youngsters primarily assist their household with part-time jobs at Ross Dress for Less.
That month, Marisol visited a Richmond department workplace of the Contra Costa County Employment and Human Services Department, hoping to talk to an eligibility employee. Instead, she was informed to go away her paperwork and to name a telephone quantity to examine her utility standing. Since then, she made quite a few calls and spent hours on maintain, however has not been capable of communicate with anybody.
County officers acknowledged longer wait occasions attributable to elevated calls and stated the typical wait time is half-hour. “We understand community members’ frustration when they have difficulty getting through at times,” spokesperson Tish Gallegos wrote in an e mail. Gallegos famous the decision middle will increase staffing throughout peak hours.
After El Tímpano reached out to the county for remark, Marisol stated she was contacted by an eligibility employee, who defined that her household was dropped as a result of their youngsters had filed taxes individually, so the Medi-Cal system decided their eligibility individually quite than as one family. The county reinstated Marisol and her household on March 15.
Marisol stated regaining Medi-Cal was a joyous however bittersweet ending to a months-long wrestle, particularly figuring out that different folks get dropped for procedural points. “Sadly, there has to be pressure for them to fix something,” she stated.
Jasmine Aguilera of El Tímpano is taking part within the Journalism & Women Symposium’s Health Journalism Fellowship, supported by The Commonwealth Fund. Vanessa Flores, Katherine Nagasawa, and Hiram Alejandro Durán of El Tímpano contributed to this text.
Medi-Cal Resources (in Spanish):
How to get insurance coverage and low-cost well being care in California
How to use for Covered California
This article was produced by KFF Health News, which publishes California Healthline, an editorially impartial service of the California Health Care Foundation.
